Pinpointing ‘what is autism spectrum disorder’ isn’t as simple as it sounds.
It can be loud. Quiet. Visible. Hidden. Joyful. Exhausting. Sometimes, it looks like brilliance in motion. Other times, it’s a complete emotional shutdown.
Curious to learn more?
Well, if you’re reading this, you’re already one step closer to understanding autism better. In this guide, we’ll explore what autism spectrum disorder (ASD) is, its causes, the signs and symptoms to watch out for, and how early intervention for autism can make a meaningful difference.
So, let’s start with the most important question of all.
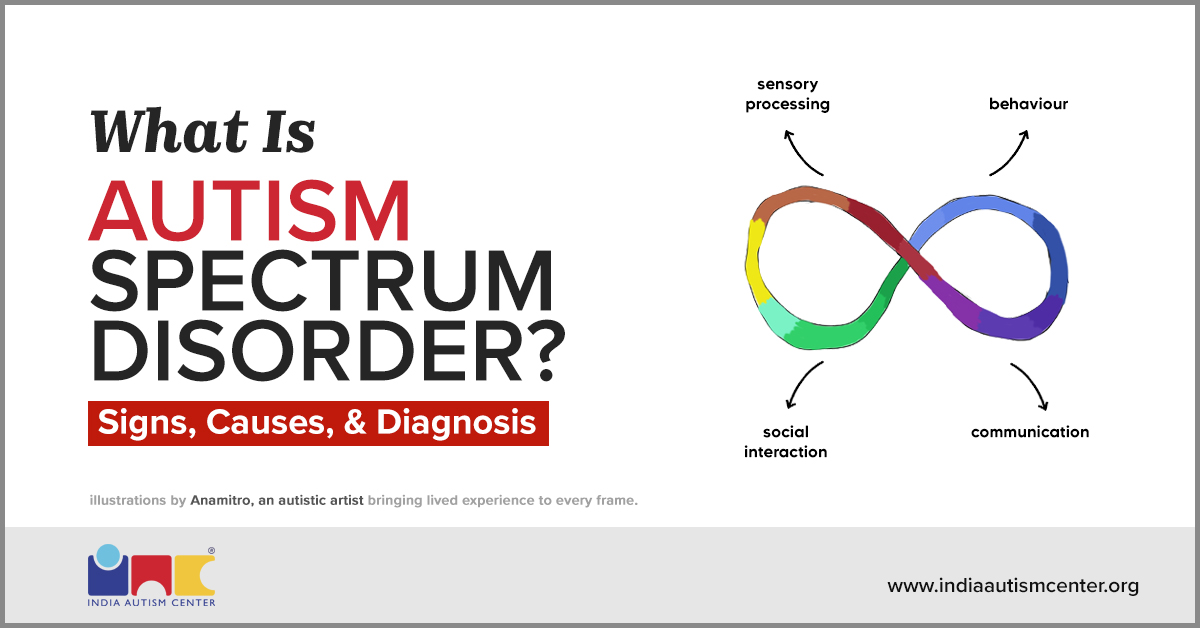
What Is Autism Spectrum Disorder?

Autism spectrum disorder is a neurodevelopmental condition that affects how a person communicates, interacts socially, and processes sensory information.
Interestingly, autism is a spectrum disorder. It doesn’t show up in just one way.
One child might talk nonstop; another might not use words at all. Some find deep comfort in routine, while others need room to explore and improvise.
Dr. Temple Grandin, one of the world’s most well-known advocates, offered a glimpse into this in her TED Talk. When asked to picture a church steeple, her mind flashed vivid images. Her classmate, however, pictured nothing.
![]()
I thought that everybody thought the same way that I think… It is where I learned how thinking can be different.
– Dr. Gradin
This is what makes autism so nuanced. It’s not always about what’s visible. It’s about how someone interprets the world internally.
So, let’s be clear. Autism is not a disease. And it certainly is not rare.
Studies estimate that it affects about 1 in 100 Indian children under the age of 10. In the USA, it is about 1 in 31 children aged 8 years.
That’s why understanding autism begins with recognizing the causes.
Let’s explore them first.
What Is Autism Caused By?

Understanding what causes autism is one of the first questions many parents ask after a diagnosis. The urge to find answers is natural. Families often retrace medical histories, revisit early signs, or reflect on emotional outbursts and delays.
But ASD doesn’t have one clear cause. Instead, it emerges from a combination of genetics, brain development, and environmental factors.
So, let’s first take a closer look at what science has to say about the causes.
Role of Genetics in Autism
Recent research estimates that genetic factors contribute to around 80% of autism risk.
Some are inherited. Others appear early in development as de novo mutations. In simpler words, these are genetic changes that occur spontaneously and aren’t passed down from parents.
These genetic variations influence how the brain forms and connects. Specifically, they impact the regions involved in communication, sensory processing, and social behavior.
Here’s where it gets interesting.
Brain Development and Autism Spectrum Disorder
As the brain develops during fetal and early postnatal life, the connections between neurons (also known as synapses) form critical pathways. This governs behavior, perception, and interaction.
In our podcast with Dr. Sumantra Chattarji, Director of CHINTA at TCG CREST, he shared,
![]()
As the brain develops in its early days, the connections between neurons don’t form in the typical fashion. As a result, the brain is wired differently over time and reaches a point where all the pieces are there. Nothing is lost. They’re just wired slightly differently.
But this also doesn’t reveal the whole picture.
Environmental and Pregnancy-Related Risk Factors Leading to Autism
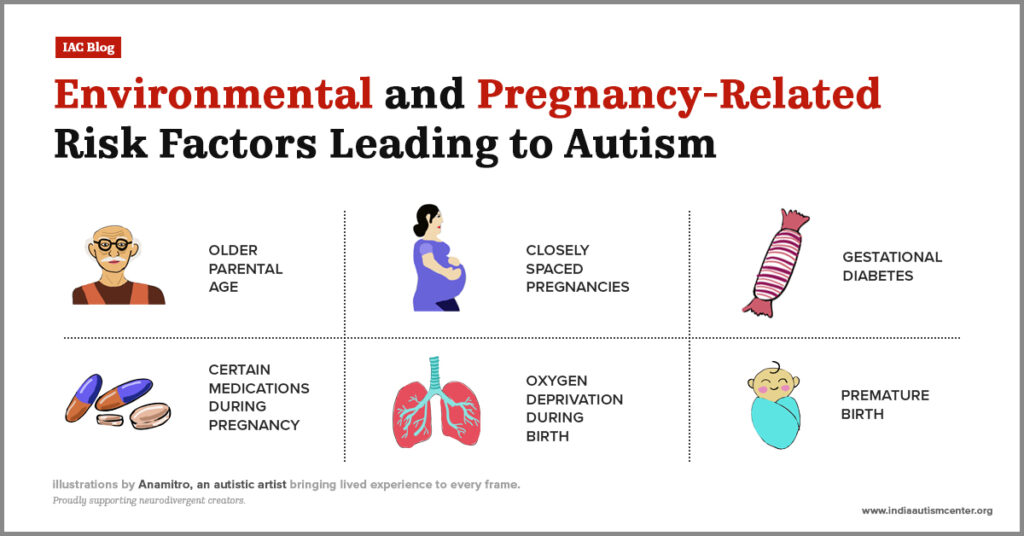
While genetics and brain development are central, researchers have also identified non-genetic risk factors that may increase the likelihood of ASD.
These include:
- Older parental age: Especially fathers over 40. This is linked to a higher likelihood of autism due to age-related genetic changes.
- Closely spaced pregnancies: Short intervals between pregnancies can affect maternal health and fetal brain development, raising the risk.
- Gestational diabetes: This condition can interfere with fetal brain development and is associated with an increased likelihood of autism in the child.
- Certain medications during pregnancy: Drugs like valproate (used to treat epilepsy) are known to disrupt fetal brain development and significantly elevate autism risk.
- Oxygen deprivation during birth: Birth complications that lead to low oxygen levels can cause brain injury, contributing to a higher risk.
- Premature birth: Babies born prematurely are more vulnerable to neurodevelopmental differences, including autism, due to early-stage brain development.
It’s important to remember that these factors do not cause ASD on their own. Instead, they may elevate risk when combined with underlying genetic susceptibility.
With that said, let’s now delve into the most-awaited aspect.
What Are Autism Symptoms and Signs?

Recognizing autism symptoms and signs is key. This helps in understanding how it’s diagnosed and how you can support someone on the spectrum.
Let’s explore what to look for.
Early Autism Symptoms and Signs In Infants (0–12 Months)
Ever wondered at what age autism is detected? For many families, subtle differences begin to appear in infancy.
Early signs of autism in infants include:
- Limited eye contact while conversing
- Rarely smiling at others or showing social interest
- Not responding to their name by 9-12 months
- Little to no babbling
- Gestures like pointing or waving
These early autism symptoms may be easy to miss. But they are crucial clues for early intervention.
Early Autism Signs and Symptoms In Toddlers (1–2 Years)
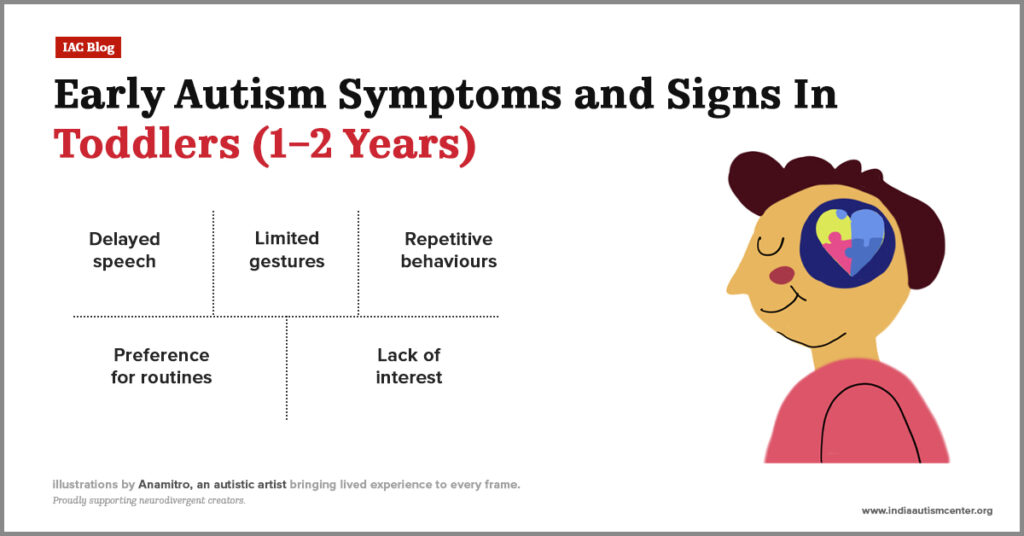
By this age, children usually begin to speak, imitate adults, and play socially. In autistic toddlers, however, development might diverge.
Watch for:
- Delayed speech or no speech by age 2
- Limited gestures like pointing, waving, or nodding
- Repetitive behaviours (rocking, flapping, spinning)
- Strong preference for routines or sameness
- Less interest in playing with others or imitating adults
This is also the stage when regressive autism can emerge.
This begs the question.
What is Regressive Autism?
Regressive autism (also called autism with regression) means the loss of previously acquired skills.
This is a subtype of ASD that is often seen in children, usually aged between 15 and 30 months.
A child who once said words, responded to their name, or enjoyed play may suddenly:
- Stop using language
- Withdraw from social interaction
- Avoid eye contact or connection
- Show reduced emotional expression
It’s important to remember that this regression is not necessarily caused by trauma or illness. It’s simply one of the ways ASD can unfold.
Early Autism Symptoms and Signs In Preschoolers (3–4 Years)
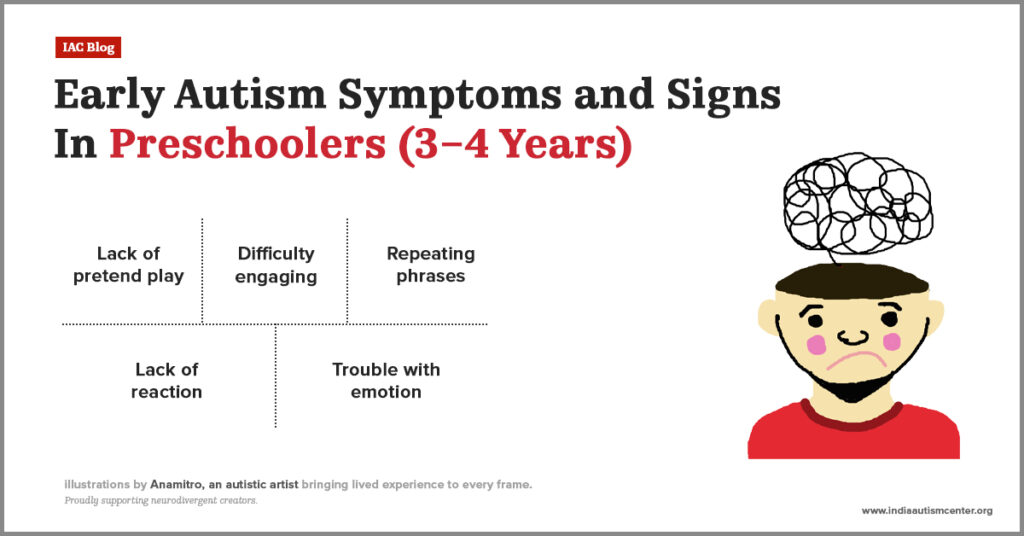
In social settings like preschool, autism signs and symptoms often become more obvious, manifesting in:
- Lack of pretend play (e.g., pretending to feed a toy)
- Difficulty engaging with peers or group activities
- Repeating phrases (echolalia) or using unusual speech patterns
- Over- or under-reaction to sounds, lights, textures
- Trouble understanding or expressing emotions
Autism Signs and Symptoms in Children and Teenagers (5–17 Years)
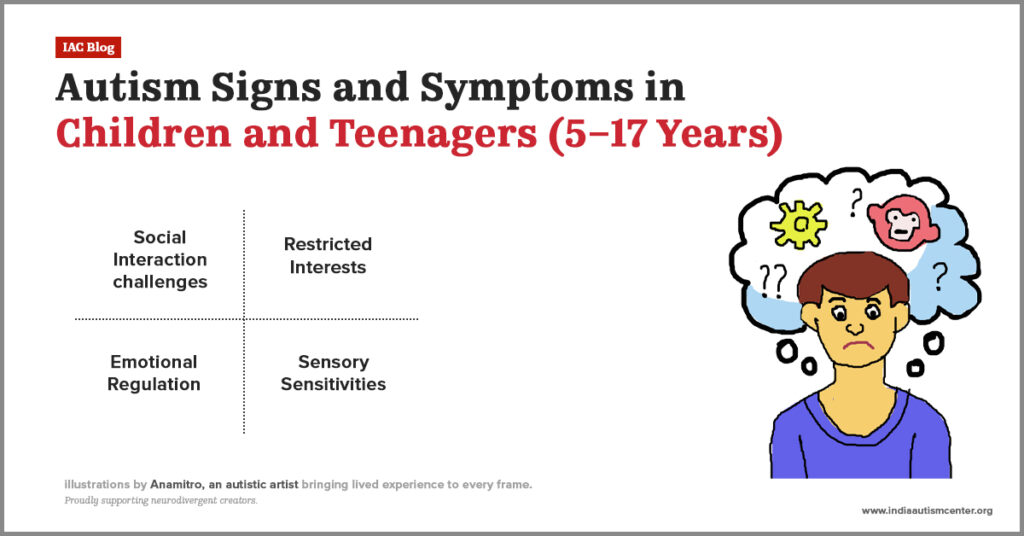
In school-aged children and teens, challenges often shift from developmental delays to social struggles, emotional regulation issues, and the effort to blend in.
Social Communication and Interaction Challenges
Navigating friendships and social expectations can become more challenging in school settings.
At this stage, autistic individuals may experience:
- Difficulty reading social cues like facial expressions, body language, or tone of voice
- Struggles with initiating or maintaining back-and-forth conversations
- Preference for playing alone or spending time with younger children or adults
- Literal interpretation of language and missing sarcasm, jokes, or implied meaning
- Limited or avoidant eye contact during conversations
Restricted Interests and Repetitive Behaviors
Autistic children and teens often develop focused interests that may dominate their time and conversations.
Common autism symptoms and signs are:
- Intense fixation on specific topics, activities, or objects
- Repetitive behaviors like spinning objects, hand-flapping, or rocking
- Insistence on routine or predictability and distress when routines are disrupted
- Difficulty transitioning between classes, tasks, or social environments
Sensory Sensitivities
Sensory differences often become more pronounced in high-stimulus environments like schools or social gatherings.
Look for:
- Overreaction to sounds, lights, or textures (e.g., buzzing lights, scratchy uniforms)
- Seeking or avoiding sensory input (e.g., covering ears, refusing certain foods)
- Overwhelm or shutdowns in crowded or chaotic spaces
Emotional Regulation and Daily Living
As expectations increase with age, autistic teens may face unique internal struggles, such as:
- Heightened anxiety, especially in social settings
- Mood changes, emotional shutdowns, or meltdowns
- Difficulty managing transitions or unexpected changes
- Trouble with daily tasks like organizing schoolwork, hygiene, or managing time
Subtle Autism Signs and Symptoms in Adulthood
In adulthood, ASD can look quieter. Traits like sensory sensitivity, social fatigue, or rigid routines often get mistaken for anxiety or just being ‘a bit different.’
Social Interaction and Communication
Part of understanding what autism is in adults is recognizing that everyday social dynamics can feel like a completely different operating system.
You might notice:
- Difficulty reading facial expressions, tone, or unspoken cues
- Preference for one-on-one conversations
- Feeling socially drained after even short interactions
- Struggling to follow fast-paced group conversations or interruptions
Routine and Change
Predictability brings comfort. A strong need for routine helps create a sense of stability in a world that feels unpredictable.
Look for:
- Discomfort with sudden changes in routine
- Deep attachment to daily rituals
- Difficulty switching between tasks
- High stress from unexpected events
- Reliance on structure to feel in control
Sensory Sensitivities
Bright lights, loud noises, or certain textures commonly trigger discomfort in adult autistic people. This makes sensory sensitivities an important yet under-recognized aspect of ASD symptoms.
These autism signs include:
- Sensitivity to bright lights, loud sounds, or strong smells
- Overwhelm in crowded or noisy environments
- Discomfort with certain textures of clothing
- Difficulty focusing due to sensory overload
Focus and Interests
Autistic adults often develop ‘special interests’. These are deep, passionate areas of focus that bring joy, clarity, and calm.
Common autism signs are:
- Intense, almost encyclopedic knowledge of certain topics
- Spending hours immersed in research or activities
- Difficulty pulling away from focused interests
- A sense of purpose rooted in specific routines or hobbies
Emotional and Internal Experience
To fully grasp autism in adulthood, you need to look beneath the surface.
Consider:
- Difficulty identifying or naming emotions (alexithymia)
- Feeling out of sync in social or emotional situations
- Chronic anxiety or burnout from masking
- Struggling to manage sensory-emotional overload
- Coping through strict routines or withdrawal
Now that we’ve explored what signs to look for, let’s talk about what to do next, especially if you’re noticing these traits in a young child.
Early Autism Identification and Intervention (Ages 0–3)
Early intervention for autism spectrum disorder is most effective when it begins before age 3.
Why? Because at this stage, the brain is rapidly developing, and children are most responsive to structured support.
If you’re wondering whether your toddler’s ‘unusual’ behavior is just a phase, don’t wait it out.
With that said, let’s now discuss the steps.
Step 1: Developmental Screening
Your first stop should be a developmental pediatrician, clinical psychologist, or rehabilitation psychologist.
Ask for a developmental screening, especially if your child is between 15 to 30 months.
Most professionals in India use the Modified Checklist for Autism in Toddlers, Revised (M-CHAT-R). It’s a reliable tool to identify early signs.
Step 2: Early Intervention
If screening raises concerns, you don’t need to wait for a formal diagnosis. Early autism intervention can begin right away.
It may include:
- Speech therapy
- Occupational therapy (OT)
- Special education support
- Parent training and home-based strategies
The goal? Prevent delays from compounding. Build communication. Nurture connection. Improve adaptive behaviors.
Autism Diagnosis in Children and Teens (Ages 3-18)
After age 3, teens and children can undergo a formal autism diagnosis. This doesn’t just confirm ASD, it also helps assess co-occurring conditions like ADHD, sensory issues, anxiety, or speech delays.
How to Get an Autism Spectrum Disorder Diagnosis
Start with a licensed clinical psychologist, rehabilitation psychologist, or developmental pediatrician.
A proper diagnosis includes:
- Parental interviews and developmental history
- Direct observation of behavior and interaction
- Review of previous therapy records or school reports
- Standardized tools like the Indian Scale for Assessment of Autism (ISAA), Indian Scale for Assessment of Autism (CARS-2), or Autism Diagnostic Observation Schedule (ADOS-2)
- A multidisciplinary team arrives at a conclusive diagnosis through consensus
Multidisciplinary Support After Diagnosis
Diagnosis is just the beginning. Based on the assessment, autistic children and teens may be referred to:
- A speech-language therapist
- An occupational therapist
- A special educator
- A psychologist
- A play therapist
- A health practitioner (for co-occurring conditions)
This integrated approach is key to designing personalized autism intervention strategies. It also truly supports the child’s strengths and challenges.
Autism Diagnosis for Adults (Ages 18+)
Not everyone receives a diagnosis in childhood. Some begin to question their lifelong struggles with communication, masking, or sensory sensitivities in adulthood.
How to Get an Autism Diagnosis as an Adult
Autism diagnosis for adults follows a similar pathway, but with added focus on lived experience and adaptive functioning.
Seek out:
- A licensed clinical or rehabilitation psychologist with experience in adult neurodevelopment
- A psychiatrist, especially if emotional or behavioral concerns like anxiety or depression are involved
They will use tools like the ISAA, ADOS-2, DISCO, or clinical interviews alongside DSM-5 autism diagnosis criteria.
The Power of Clarity
Receiving a diagnosis in adulthood helps explain long-standing challenges and opens doors to support, workplace accommodations, and therapy.
It also helps uncover any co-occurring conditions that may have been misunderstood.
As Puja Dutta, an RCI-licensed Clinical Psychologist at India Autism Center, shared:
![]()
Ethical diagnosis isn’t just about a label. It’s about understanding the child or adult, and building interventions that work in real life.
Caution: Avoid Online or Remote Diagnosis
While preliminary consultations can happen online, a proper diagnosis must be done in person.
Tools like ISAA and ADOS-2 rely on live behavioral cues, eye contact, gestures, and shared attention. These are not reliably captured over video.
Always seek in-person assessments through certified professionals.
Now, here is something to keep in mind.
Co-occurring Conditions in Autism Spectrum Disorder
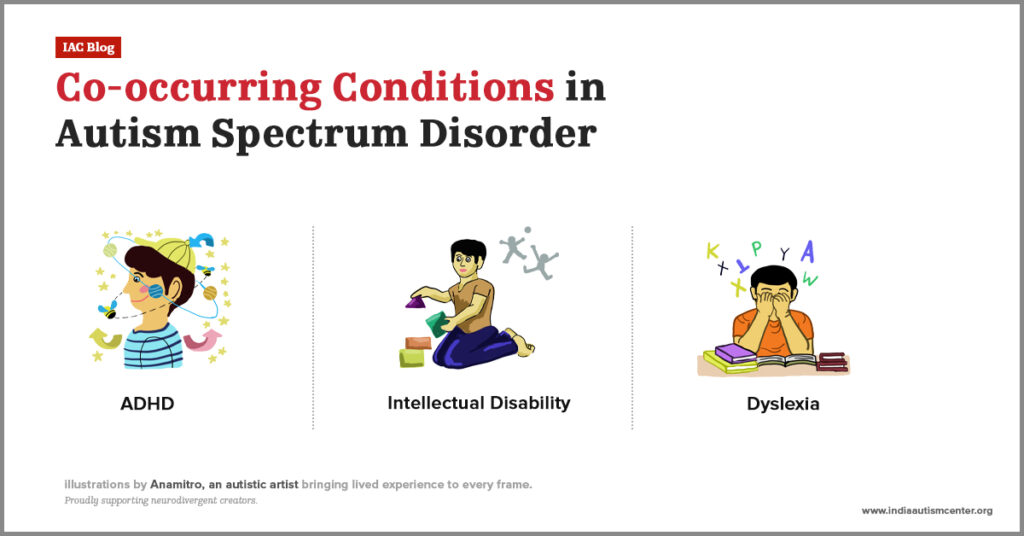
Many autistic individuals experience other neurodevelopmental, medical, or psychological conditions alongside their autism diagnosis. These are called co-occurring conditions.
Recognizing them is vital for delivering the right support. Here are the most common ones:
Attention-Deficit/Hyperactivity Disorder (ADHD)
Frequently co-occurring with autism, ADHD includes symptoms like inattention, impulsivity, and hyperactivity. It can increase sensory overwhelm and make routines more difficult to follow.
Intellectual Disability (ID)
Some autistic individuals have below-average intellectual functioning, qualifying as having intellectual disabilities. This impacts their learning pace, communication, and adaptive living skills.
Dyslexia
This reading-related difference may go unnoticed in verbal autistic individuals. But becomes unavoidable to address because dyslexia causes major frustration in language-heavy learning environments.
Gastrointestinal (GI) Issues
A complete understanding of ASD must include the gut-brain connection. In other words, gastrointestinal issues accompany autism.
Chronic GI concerns, like constipation, stomach pain, or food sensitivities, often impact behavior, mood, and focus.
Fibromyalgia
In autistic adults, fibromyalgia may present as chronic pain and fatigue, further intensifying sensory sensitivities and emotional stress.
Selective Mutism
Selective mutism is an anxiety-related condition. It makes situations extremely difficult for some autistic children to speak in certain settings, even when they want to.
Sensory Processing Differences
Sensory sensitivities are a core trait. It includes extreme responses to light, sound, touch, or smell. Sensory processing differences can interfere even with daily tasks like dressing, eating, or relieving oneself.
Epilepsy
Seizures occur more frequently in autistic individuals, especially those with intellectual disabilities. If this is epilepsy, seizures can begin in early childhood or develop later during adolescence.
Psychosis
Though rare, some autistic individuals may show signs of psychosis. Psychotic episodes involve experiences of hallucinations or delusions, usually linked to stress, trauma, or genetic vulnerability.
Developmental Coordination Disorder (DCD)
Often seen in autistic children, developmental coordination disorder affects fine and gross motor skills. DCD leads to clumsiness or difficulty with handwriting, sports, or dressing.
Obsessive Compulsive Disorder (OCD)
Obsessive-compulsive disorder and ASD can look similar. However, OCD is primarily driven by anxiety and intrusive thoughts, requiring different interventions.
Polycystic Ovary Syndrome (PCOS)
Autistic women and girls are more prone to having PCOS. This suggests that hormonal pathways may play a role in how autism is expressed and experienced.
All of these co-occurring conditions may stay hidden well into adulthood. Not because they weren’t there. But because individuals often mask them to get through the day.
This raises the question.
What is Masking in Autism?

Autism masking, also known as camouflaging or compensating, is a social strategy where autistic individuals hide parts of themselves to blend in with a world that doesn’t always make room for difference.
It might look like this:
- Forcing eye contact even when it feels unnatural
- Suppressing stimming, like rocking, hand-flapping, or tapping, because someone once said it looked odd
- Rehearsing conversations ahead of time to sound ‘normal’
These strategies often work. Sometimes, they even help autistic individuals get through the day. Help them feel safe. Accepted. And, avoid being teased.
Another way autism gets misunderstood is through the language we use, especially when it comes to describing ability levels.
So, let’s talk about them.
What is the Difference Between High and Low Functioning Autism?

You’ve probably heard terms like high functioning autism or low functioning autism in casual conversations. Maybe even in some diagnostic reports.
So, it’s quite natural to wonder what these terms mean.
What is High Functioning Autism?
High functioning autism refers to autistic individuals who:
- Use spoken language fluently
- Perform well in school or work
- Appear socially typical at first glance
But here is the catch.
Many high functioning autistic individuals deal with daily challenges that go unnoticed. Often, because they’re good at masking them.
However, beneath the surface, there’s:
- Sensory overload that builds up silently
- Struggles with social communication and expectations
- Anxiety, shutdowns, or burnout from constant self-monitoring
Now let’s discuss the opposite label.
What is Low Functioning Autism?
The individuals with low functioning autism:
- Have little or no spoken language
- Need high levels of daily living support
- May have co-occurring intellectual disability
- Face significant barriers in traditional communication or schooling
But what it doesn’t reflect are:
- Nonverbal intelligence or pattern recognition
- Deep emotional insight or visual/spatial strengths
- The ability to connect, express, and learn, just differently
So, as it turns out, the word ‘functioning’ flattens the picture.
What’s the Alternative?
Terms like ‘functioning’ flatten a complex spectrum. Instead, clinicians now describe autism using support levels, as per DSM-5 autism diagnosis criteria:
- Level 1: Requires support
- Level 2: Requires substantial support
- Level 3: Requires extremely substantial support
This approach respects individuality and focuses on the real question: What support does the person need to thrive?
Now, just as important as understanding what autism is, we must also understand what it is not.
What Are Some Common Autism Myths and Misconceptions?

From news stories to Netflix shows, ASD is often shown in narrow, predictable ways. The quirky genius. The emotionless coder. The one who ‘just doesn’t get people’.
But ASD doesn’t come in one template. These repeated portrayals can erase the real-life diversity of experiences among autistic individuals.
We will now set the record straight about autism myths and facts.
Myth 1: Autism Is A Disease
Truth: Autism spectrum disorder is not a disease. It’s a lifelong neurodevelopmental condition.
Myth 2: Autism Is A Mental Illness
Truth: ASD is not a psychiatric disorder. However, co-occurring conditions like anxiety or depression are common.
Myth 3: There’s an Autism Epidemic
Truth: Higher diagnosis rates are due to better awareness and broader criteria.
Myth 4: Only Boys Can Be Autistic
Truth: Signs of autism in women are often subtle. In most cases, they are underdiagnosed due to social masking and gender bias in diagnostic tools.
Myth 5: Autistic People Are Either Nonverbal or Geniuses
Truth: The autism spectrum is wide. Some are non-verbal; others are hyper-verbal. Sensitivities, support needs, and strengths vary widely. One person’s traits don’t represent the whole spectrum.
Myth 6: Vaccines Cause Autism
Truth: There is no scientific evidence linking vaccines and autism spectrum disorder. This myth originated from a retracted and fraudulent study. Multiple global studies have confirmed that vaccines do not cause autism.
Myth 7: Bad Parenting Causes Autism
Truth: This outdated autism myth has been debunked. Parenting style does not cause autism.
Myth 8: Autism Can Be Cured
Truth: Autism is not something to be cured. Instead, the goal should be to provide individualized support.
Myth 9: Autistic People Can’t Live Independently
Truth: Some individuals on the spectrum need high levels of support; others live fully independent lives. That is why success looks different for each person living with autism.
Your Role Supporting Autistic People with Understanding

Autism support starts by creating a space where an autistic person feels safe, understood, and truly seen.
When the world feels overwhelming, a calm and predictable environment can ease sensory overload, reduce anxiety, and foster a sense of belonging.
Support isn’t just for childhood. It matters across the lifespan of individuals on the spectrum. From early intervention to adult care, consistent understanding and accommodations can make a lifelong difference.
So, how can you help?
Here are our practical tips for autism care:
- Build reliable routines that bring comfort and structure
- Tune into sensory needs, dim harsh lights, reduce noise, and offer quiet corners
- Communicate clearly and patiently, respecting individual preferences and communication styles
For those ready to support professionally, structured learning makes all the difference. For instance, our Primary Support Staff (PSS) training program offers hands-on knowledge and tools to care for individuals on the spectrum with empathy, skill, and confidence.
So, if you’re ready to start your journey in autism care, contact us now.
Frequently Asked Questions
How do I know if my child has autism?
There’s no single test, but here are some early signs to look for:
- Limited eye contact or social engagement
- Delayed speech or minimal gestures
- Repetitive movements like rocking or hand-flapping
- Intense reactions to textures, sounds, or routine changes
- A strong preference for playing alone
If these patterns persist, speak with a developmental pediatrician or clinical psychologist. Early intervention for autism can significantly improve long-term outcomes.
Can autism be cured or treated?
ASD is not something to be cured. It’s a different way of being. However, therapy, communication support, and structured routines can help build skills and reduce challenges.
Can autism improve with age?
Traits may evolve or become easier to manage, especially with early support. But autism is lifelong. What can grow is confidence, emotional regulation, and self-advocacy.
At what age is autism usually diagnosed?
Autism can often be identified by 18–24 months. But most diagnoses in India happen between the ages of 2 and 4. In some cases, especially when traits are masked, adult autism diagnosis may occur later in life.
What is the difference between autism and dementia?
Autism is present from early life and involves different sensory and social processing. Dementia, on the other hand, is a degenerative condition that leads to memory loss and cognitive decline, typically in older adults.
What is the difference between autism and Asperger’s disorder?
Asperger’s was once used to describe autistic individuals with strong verbal skills and no cognitive delays. Today, it’s folded into autism spectrum disorder under the DSM-5. The term is outdated in clinical settings.
What is severe autism?
Severe autism generally refers to individuals who have limited or no verbal language, co-occurring intellectual disability, and high support needs. It often aligns with Level 3 autism under DSM-5 classification.
What is the difference between autism and ADHD?
While both can include inattention and impulsivity, autism affects social communication and sensory regulation. ADHD is more focused on attention span, hyperactivity, and impulse control. The two can co-occur, but they’re distinct conditions.
What is the difference between autism and Down syndrome?
Autism affects how the brain processes social and sensory input. Down syndrome is a genetic condition (trisomy 21) with distinct physical and cognitive features. Some individuals have both, but they are entirely separate diagnoses.
What is the difference between autism and mental retardation?
Intellectual disability (formerly known as mental retardation) involves significant limitations in cognitive function and adaptive behavior. While some autistic individuals have intellectual disabilities, many do not.
What is borderline autism?
Borderline autism is a non-clinical term. It is sometimes used when a person shows autistic traits but doesn’t meet full diagnostic criteria. These individuals may still benefit from support.
What is atypical autism?
Atypical autism was used to refer to those with some but not all traits of autism. It’s important to note that this is no longer a formal diagnosis.
What is considered nonverbal autism?
Nonverbal autism means a person on the spectrum doesn’t use spoken words to communicate, or uses very few. They might use gestures, sounds, pictures, or devices instead. This is different from being nonverbal due to things like trauma or illness. Here, the brain develops differently, making speech hard to learn or use naturally.