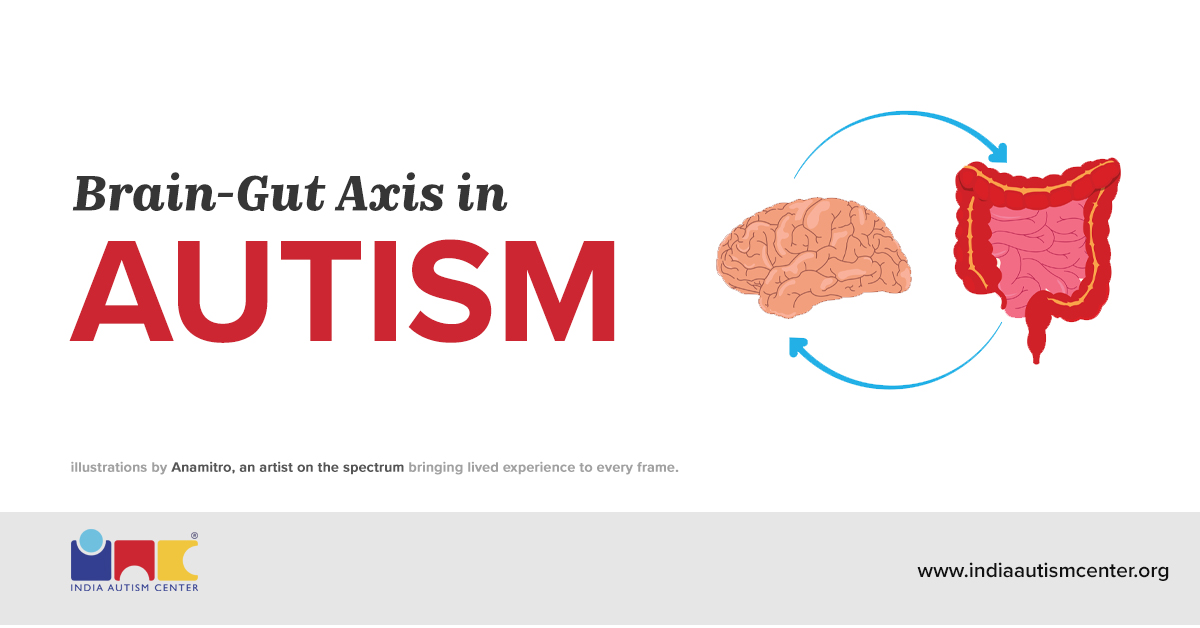
When we talk about autism today, we usually think about the brain — communication challenges, social interactions, and behaviour differences. But what if I told you that your brain isn’t acting alone? Yes, the Brain-Gut Axis in autism spectrum disorder (ASD) is one of the most talked-about connections in neuroscience and nutrition right now.
It represents a two-way communication highway between your gut and your brain. This connection may help explain why so many individuals with autism also have digestive problems — and why targeting gut health could become an essential part of improving quality of life.
Let’s explore it piece by piece, in a clear, easy-to-understand way.
What Is the Brain-Gut Axis?
The Brain-Gut Axis in autism refers to a constant flow of signals between your nervous system and your gastrointestinal (GI) system. Scientists call this interaction the microbiota-gut-brain axis in autism spectrum disorder. It isn’t just metaphorical — it’s a biological system, involving nerves, chemicals, and immune signals.
In simple terms: Your gut talks to your brain — and your brain talks back.
Here’s how:
- Your Enteric Nervous System (ENS) — millions of neurons in the gut, actually works alongside your central nervous system.
- The vagus nerve is like a superhighway transmitting signals between the gut and the brain.
- Your gut produces key neurotransmitters — including about 90% of the body’s serotonin — which affects mood and behaviour.
This means that changes in your gut can literally influence brain chemistry and vice versa.
Why the Gut Matters in Autism
Let me be direct with you: many autistic individuals experience gastrointestinal symptoms such as constipation, diarrhoea, abdominal pain, and bloating at much higher rates than others. Research finds that up to 70% of children with autism have some form of GI dysfunction.
But the connection goes beyond discomfort. Studies on the microbiota-gut-brain axis in autism spectrum disorder show that:
- The balance of gut bacteria (your microbiota) can influence behavioural symptoms.
- When gut bacteria are imbalanced (dysbiosis), immune, neural, and hormonal pathways may be affected.
- Dysbiosis also increases gut permeability (“leaky gut”), which may allow inflammatory molecules to impact the brain.
This is why addressing the Brain-Gut Axis in autism isn’t just about soothing tummies — it’s about improving communication between body and brain.
Want to know more? Get in touch with us.
Gut Bacteria and Autism: What the Science Says
Now let’s talk about gut microbes. When people say “good bacteria,” they’re referring to tiny organisms living in your gut that help break down food, produce chemicals, and protect against bad microbes.
Your gut microbiota affects:
- Neurotransmitters (chemicals like serotonin and GABA)
- Immune signaling
- Metabolites (small molecules) that travel to the brain
These microbial changes may:
- Influence short-chain fatty acid (SCFA) production — vital players that help maintain gut lining and brain health.
- Affect neurotransmitter synthesis and immune responses.
It’s important to understand this isn’t claiming that gut bacteria cause autism. Autism is complex — involving genetics, environment, and early development. But their connection suggests that gut health influences how symptoms show up and could become a real target for care.
Early Life and Microbiome Development
From the moment you were born, your gut microbiota started forming. In fact:
- Microbial colonisation begins before birth — even in amniotic fluid and placenta.
- Delivery mode (vaginal vs. cesarean) affects early microbiota.
- Breastfeeding transfers beneficial bacteria.
By around age three, your gut microbiota becomes relatively stable, and this is exactly when the brain is rapidly developing. A baby’s brain goes from about 36% to 90% of adult volume by age two — a period where gut and brain development are deeply intertwined.
So, when early gut balance is disrupted by antibiotics, diet patterns, or infections, the microbiota-gut-brain axis in autism spectrum disorder may be affected.
Antibiotics, Dysbiosis, and Development
Antibiotics can save lives. But they don’t know the difference between “good” and “bad” bacteria. Especially in early childhood, repeated antibiotic use can:
🔹 Disrupt gut microbiota balance
🔹 Reduce beneficial bacteria
🔹 Increase microbial imbalance (dysbiosis)
A 2018 study found that about 34.5% of children with autism had repeated exposure to broad-spectrum antibiotics early in life, compared to controls.
Such disruption may ripple through the Brain-Gut Axis in autism, contributing to behavioural and neurological differences. We need more research, but the evidence suggests that mindful antibiotic use in early life matters.
Want to know more? Get in touch with us.
Could Gut Bacteria Help Treat Autism?
Now that we’ve laid the foundation, let’s talk about gut bacteria autism treatment — what’s promising and what’s still emerging.
Probiotics and Prebiotics
- Probiotics introduce beneficial strains of bacteria.
- Prebiotics are food for those good bacteria (think fibre).
Early evidence shows that probiotics and prebiotics may help reduce gastrointestinal symptoms and support mood and behaviour.
Dietary Approaches
Certain diets (e.g., high-fibre, antioxidant-rich, gluten-free) may improve gut microbiota composition and reduce inflammation.
These approaches aim to support the gut, which in turn may help regulate the brain via the microbiota-gut-brain axis.
Faecal Microbiota Transplant (FMT)
FMT — also called Microbial Transplant Therapy — transfers a healthy gut microbiome from a donor. This therapy has shown promising early results in restoring microbial balance and improving GI symptoms.
Here is a detailed article on the Autism Diet: A Detailed Guide (2026).
What the Research Says: Cautious Optimism
Scientists are enthusiastic but cautious. Studies in medical journals consistently show a bidirectional influence between gut microbes and brain pathways — but they also stress that autism is not solely caused by the microbiota.
Rather, the microbiota-gut-brain axis in autism spectrum disorder likely plays a role in:
- Severity of symptoms
- GI challenges
- Behavioral responses
- Immune and metabolic regulation
Researchers are now moving toward personalised treatments that consider who might benefit most from gut-focused therapies.
Practical Tips You Can Use Today
If you want to support the Brain-Gut Axis in autism, here are some steps that many nutritionists and clinicians recommend:
Focus on Gut-Friendly Foods
- Whole foods
- High-fibre vegetables
- Fermented foods (yoghurt, kefir, sauerkraut)
These feed beneficial bacteria, a key part of gut bacteria autism treatment.
Minimise Unnecessary Antibiotics
Work with a doctor to weigh the benefits and impacts, especially in young children.
Try Probiotics and Prebiotics
Under supervision, supplements may help balance microbiota.
Track Symptoms
Keeping a food and behaviour journal can help you connect diet changes with improvements.
Want to know more? Get in touch with us.
Effect of Antibiotics on Autism Spectrum Disorder
A human’s microbiome develops from birth until the age of 3. Using antibiotics during these formative years can influence the development of metabolic and neurological conditions. Antibiotics can seriously impact the gut’s microbial composition by disrupting the growth of pathogenic microbes. Early and excessive use of antibiotics can lead to microbial dysbiosis, which may play a role in the development of autism.
This affects the gut-brain axis. It can lead to epigenetic changes, potentially influencing the development of autism. A recent study showed that autism behavioural symptoms and gut health are most definitely linked.
A 2018 study by Eshraghi found that 34.5% of autistic children had been exposed to extensive and repeated use of broad-spectrum antibiotics. It was more than six courses compared to a control group with more than six courses.
Conclusion
If you’re living with autism or caring for someone who is, I want you to come away with this:
The Brain-Gut Axis in autism connects the stomach and the brain in ways we’re still learning. By caring for the gut — through nutrition, lifestyle, and evidence-based therapies — you might support better overall health and behaviour.
This isn’t a cure. But it is a hopeful piece of the bigger puzzle.
If you want to explore gut bacteria autism treatment options, talk to a clinician who understands both neurological and digestive systems — because when the gut and brain cooperate, you may just see real improvements.
Frequently Asked Questions (FAQs)
What is the Brain-Gut Axis in autism?
The Brain-Gut Axis in autism refers to the two-way communication between the gut and the brain through nerves, hormones, immune signals, and gut bacteria. In individuals with autism, this connection may function differently, which can explain why gastrointestinal issues and behavioral challenges often occur together.
How does gut bacteria affect autism symptoms?
Gut bacteria play a key role in producing neurotransmitters, regulating inflammation, and supporting immune health. Imbalances in gut microbes may influence behavior, mood, and digestion. This is why gut bacteria autism treatment approaches, such as probiotics and diet changes, are being actively researched.
Can improving gut health help manage autism?
Improving gut health may help reduce gastrointestinal discomfort and support overall well-being in some individuals with autism. While it is not a cure, supporting the microbiota-gut-brain axis in autism spectrum disorder through diet, probiotics, and medical guidance may help manage certain symptoms.
Are probiotics and diet changes safe for autism?
In most cases, probiotics and gut-friendly diets are considered safe when used under medical supervision. However, every individual with autism is unique. It’s important to consult a healthcare professional before starting any gut bacteria autism treatment to ensure it suits specific needs.
For expert insights, support services, and inclusive learning initiatives, visit the India Autism Center.