If you are the parent of a child with special needs, you carry a weight that most other parents don’t. You think about tomorrow, next year, and decades from now. You worry about who will care for your child when you are no longer around. These thoughts can keep you awake at night.
This guide is here to help you turn those worries into a plan. Financial planning for a child with special needs is not just about money. It is about love, security, and peace of mind. It is about ensuring that your child’s future is safe, dignified, and happy, no matter what.
We have taken expert advice and broken it down into simple, actionable steps. Everything is written from an Indian perspective, using Indian terms, and keeping Indian families and their unique challenges in mind.
Part One: Understanding Your Responsibility
The Two-Lifetime Reality
In a typical Indian family, parents work hard, save money, and hope their children will grow up, get jobs, get married, and support them in their old age. The financial plan is simple: earn, save, spend on children’s education and marriages, and then retire.
Your situation is different. Your child with special needs may always need some level of support. They may never be able to earn a full income or manage money independently. This means your financial plan must cover not just your own lifetime, but your child’s entire lifetime after you.
This is called Two-Generation Planning:
- Your lifetime: The years you are earning, saving, and directly caring for your child.
- Your child’s lifetime (after you): The decades when your child will need financial support from the assets you leave behind.
This is a big responsibility, but it is not impossible. Thousands of Indian parents have done it. You can too.
Have the Difficult Conversations
Before you open any bank account or buy any insurance policy, you must sit down with your spouse and family and have an honest conversation.
Questions to Discuss:
- Who will care for our child if something happens to both of us?
- Are our parents, siblings, or other relatives willing and able to take on this responsibility?
- How much money will our child need each month for the rest of their life?
- Where will our child live as an adult? With family? In a group home? In supported living?
These conversations can be emotional. That is okay. But do not avoid them. Talking openly is the first step toward building a secure future.
Part Two: Know Your Numbers
Track Every Rupee You Spend Today
You cannot plan for the future if you do not understand your present. The first practical step is to write down exactly what you spend every month.
Get a notebook or open a simple spreadsheet. Write down:
- Household Expenses:
- Rent or home loan EMI
- Groceries and food
- Electricity, water, gas, internet bills
- Transport (fuel, auto, bus, train)
- Mobile phone and entertainment
- Child’s Care Expenses:
- School fees (special school or inclusive school)
- Therapy costs (speech therapy, occupational therapy, physiotherapy, behavioural therapy, counselling)
- Medicines, supplements, and doctor visits
- Therapist travel costs (if they come home)
- Special equipment (hearing aids, glasses, mobility aids, communication devices)
- Support Staff Expenses:
- Salary for a nanny, caregiver, or personal assistant
- Any training costs for caregivers
- Miscellaneous:
- Clothing and personal items for your child
- Hobbies, activities, and outings
- Any alternative therapies or treatments
Want to know more? Get in touch with us.
Why This Matters:
You cannot know how much to save for the future if you don’t know how much you spend today. This exercise also helps you spot areas where you might be able to save a little.
Imagine Your Child’s Future Needs
Now, think ahead. Your child’s needs will change as they grow. Try to imagine what their life might look like at different stages.
Age 0-10 Years:
- Focus on early intervention, therapy, and special education.
- Expenses: Therapies, specialists, school, equipment.
Age 10-18 Years:
- Focus on life skills, social skills, and transition planning.
- Expenses: Continued therapy, vocational training, assistive technology, and possibly a personal assistant.
Age 18-30 Years:
- Focus on adulthood, day programs, supported employment, or sheltered workshops.
- Expenses: Day centre fees, job coach, continued therapy, social activities.
Age 30+ Years:
- Focus on long-term care, housing, and quality of life.
- Expenses: Supported living or residential care, full-time carers, medical care, leisure activities.
For Each Stage, Ask Yourself:
- Where will my child live?
- Who will care for them?
- What will they do during the day?
- What medical and therapy needs will they have?
- How much will all of this cost at today’s prices?
This is not about predicting the future perfectly. It is about thinking ahead so you can plan.
Part Three: Building Your Financial Foundation
Create Your Emergency Fund (Your First Priority)
Before you invest in anything, before you think about the stock market, you must build an emergency fund. This is the most important financial step you will take.
What is an Emergency Fund?
It is a pot of money set aside ONLY for unexpected emergencies. Not for a new TV. Not for a family wedding. Only for true crises.
Why Do You Need One?
Children with special needs can have unpredictable health issues. Therapies may need to be added suddenly. A caregiver may quit. You may lose your job. Your emergency fund ensures that when life throws a curveball, you do not have to sell your investments or borrow money at high interest rates.
How Much Should You Save?
Aim for 6 to 12 months of your TOTAL monthly expenses (everything you wrote down in Chapter 3). If your family spends ₹50,000 per month, your emergency fund target is ₹3,00,000 to ₹6,00,000.
Where to Keep It:
This money must be SAFE and EASILY ACCESSIBLE. Do not invest it in the stock market.
Keep it in:
- A savings bank account (preferably one with decent interest)
- A liquid mutual fund (very safe, can be withdrawn in 1-2 days)
- Fixed deposits with easy withdrawal options
How to Build It:
- Set up an automatic monthly transfer from your salary account to a separate savings account.
- Start small. Even ₹500 or ₹1000 a month adds up over time.
- Do not touch this money for anything other than real emergencies.
Want to know more? Get in touch with us.
Understand Your Investments
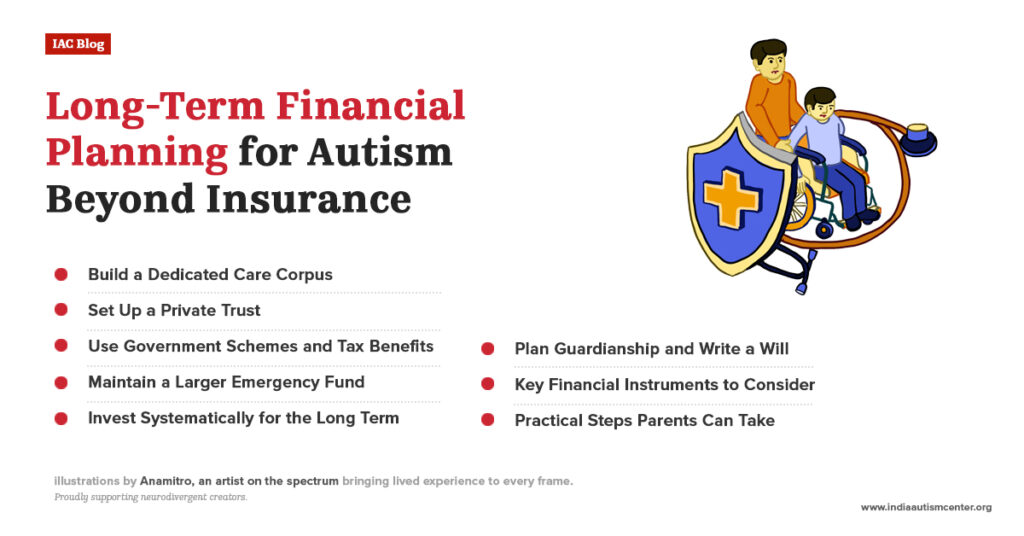
Once your emergency fund is in place, you can start thinking about long-term investments. This is the money that will grow over decades and eventually support your child.
The Problem with Keeping All Money in Fixed Deposits:
Many Indian parents feel safe keeping all their money in Fixed Deposits (FDs), PPF, or savings accounts. This feels safe because the money does not lose value in rupees. But it does lose value in what it can BUY. This is called inflation.
What is Inflation?
In simple words, prices go up every year. A ₹100 therapy session today may cost ₹200 in 10 years. If your money only grows at 5% in an FD, but inflation is 6%, you are actually losing purchasing power.
To beat inflation, you need some investments that can grow faster than inflation.
Investment Options in India:
- For Short-Term Needs (0-3 Years):
- Savings Account
- Liquid Mutual Funds
- Short-Term Fixed Deposits
- For Medium-Term Needs (3-10 Years):
- Debt Mutual Funds
- Balanced Mutual Funds (mix of debt and equity)
- Fixed Maturity Plans (FMPs)
- Recurring Deposits (RDs) for disciplined saving
- For Long-Term Needs (10+ Years):
- Equity Mutual Funds (Stocks): These are essential for long-term growth. They can go up and down in the short term, but over 10-20 years, they have historically given much higher returns than FDs.
- Options: Large-cap funds (safer), Mid-cap funds (higher risk), Small-cap funds (highest risk), Index funds (simple, low-cost).
- Public Provident Fund (PPF): Very safe, tax-free, but the money is locked for 15 years. Good for very long-term, safe savings.
- Sukanya Samriddhi Yojana (if you have a daughter): Excellent interest rate and tax benefits.
- National Pension System (NPS): Good for retirement planning, with tax benefits.
- Direct Stocks: Only if you have the knowledge and time to research.
- Equity Mutual Funds (Stocks): These are essential for long-term growth. They can go up and down in the short term, but over 10-20 years, they have historically given much higher returns than FDs.
A Simple Investment Approach:
- Do not try to get rich quick. Avoid tips and shortcuts.
- Invest every month through a Systematic Investment Plan (SIP) in mutual funds.
- Choose 2-3 good diversified equity funds for long-term growth.
- Increase your SIP amount every year as your income grows.
- Be patient. Let compounding do its magic.
What is Compounding?
Think of it like a snowball rolling down a hill. It starts small, but as it rolls, it picks up more snow and grows bigger and bigger. With investing, your money earns returns. Those returns earn returns. Over time, the growth becomes exponential.
Example:
If you invest ₹5,000 per month in an equity fund that gives an average 12% return per year:
- In 10 years, you will have about ₹11.5 lakhs.
- In 20 years, you will have about ₹50 lakhs.
- In 30 years, you will have about ₹1.76 crores.
This is the power of starting early and staying consistent.
Want to know more? Get in touch with us.
Insurance – Your Safety Shield
Insurance is not an investment. It is protection. It ensures that if something happens to you, your child’s future is not destroyed.
Types of Insurance You Need:
- Term Life Insurance (Essential):
- This pays a large lump sum to your family if you die during the policy term.
- It is the cheapest and purest form of life insurance.
- How much do you need? Calculate the total amount your child will need for their lifetime. This could be ₹1 crore, ₹2 crores, or more. Buy term insurance for that amount.
- Important: Buy term insurance from a reputable company. Do not mix it with investment plans (like ULIPs or money-back policies) unless you have fully understood them and have a specific need.
- Health Insurance (Essential):
- Medical costs in India are rising fast. A single hospitalisation can wipe out years of savings.
- Buy a comprehensive health insurance policy for yourself, your spouse, and your child.
- For your child with special needs: Be very careful. Read the policy wording to understand what is covered and what is excluded. Some policies may exclude pre-existing conditions or certain treatments. You may need to look for specialised policies or be prepared to cover some costs out-of-pocket.
- Consider a “super top-up” plan for additional coverage at a lower cost.
- Critical Illness Insurance:
- This pays a lump sum if you are diagnosed with a specified critical illness (like cancer, heart attack, stroke).
- This money can be used for treatment, for modifying your home, or for hiring extra care for your child while you recover.
- Personal Accident Insurance:
- Provides coverage in case of accidental death or disability.
A Note on Insurance for Your Child:
In India, it is difficult to get comprehensive health insurance that fully covers all the needs of a child with special needs. This is a reality you must accept. Your financial plan must include a significant amount of money set aside specifically for future medical expenses. Insurance is a help, but it is not a complete solution.
Part Four: Legal and Estate Planning
Write a Will – It Is Not Optional
If you die without a will (called dying “intestate”), Indian law decides who gets your property. For a child with special needs, this can be a disaster. Your assets could go to relatives who may not care for your child as you would wish. There could be disputes. Your child could be left with nothing.
What a Will Allows You to Do:
- Decide exactly who gets your property and money.
- Appoint a guardian for your child (if they are minors).
- Appoint trustees to manage money for your child’s benefit.
- Create a trust within your will to protect your child’s inheritance.
You must consult a lawyer to write a proper will. Do not use a “will kit” or try to do it yourself.
Appoint Guardians and Trustees
Guardian: A guardian is the person who will take physical care of your child if you die while your child is still a minor (under 18). Choose someone who:
- Loves your child.
- Is willing and able to take on this responsibility.
- Is likely to be alive and healthy for many years.
- Shares your values and beliefs about care.
Discuss this with the person before naming them in your will.
Trustees: A trustee is a person or an institution (like a bank or a trust company) that will manage the money you leave for your child. This is especially important if your child cannot manage money themselves. You can set up a Private Trust specifically for your child’s benefit. The trust holds your assets, and the trustees use the money to pay for your child’s care according to your instructions.
You can appoint:
- Family members you trust.
- Close friends.
- A professional trustee (like a chartered accountant or a lawyer).
- A corporate trustee (like a bank’s trust department).
Having both a loving guardian and financially responsible trustees ensures your child is cared for personally and financially.
Write a Letter of Intent
This is not a legal document, but it is priceless. It is a letter to your child’s future caregivers, explaining everything they need to know.
What to Include:
- About Your Child: Their personality, likes, dislikes, routines, fears, and joys. What makes them laugh? What calms them when they are upset?
- Daily Life: Morning routine, meal preferences, bathroom needs, bedtime routine.
- Communication: How does your child communicate? Do they use words, signs, pictures, or a device? What do different sounds or behaviours mean?
- Medical Information: Diagnoses, allergies, medications, doctors, hospitals.
- Care Needs: Detailed instructions on personal care, supervision needs, and any special handling.
- Education and Day Activities: What does your child enjoy doing? What programs do they attend?
- Important People: Names and contact details of family, friends, therapists, and anyone important in your child’s life.
- Financial Information: Details of the trust, bank accounts, insurance policies, and benefits.
- Your Hopes and Wishes: What kind of life do you dream of for your child? What values do you want their caregivers to uphold?
Keep this letter with your will and update it every few years.
Want to know more? Get in touch with us.
Part Five: Government Benefits and Support in India
The Indian government and various state governments have schemes to support persons with disabilities and their families. These benefits can be a crucial part of your financial plan.
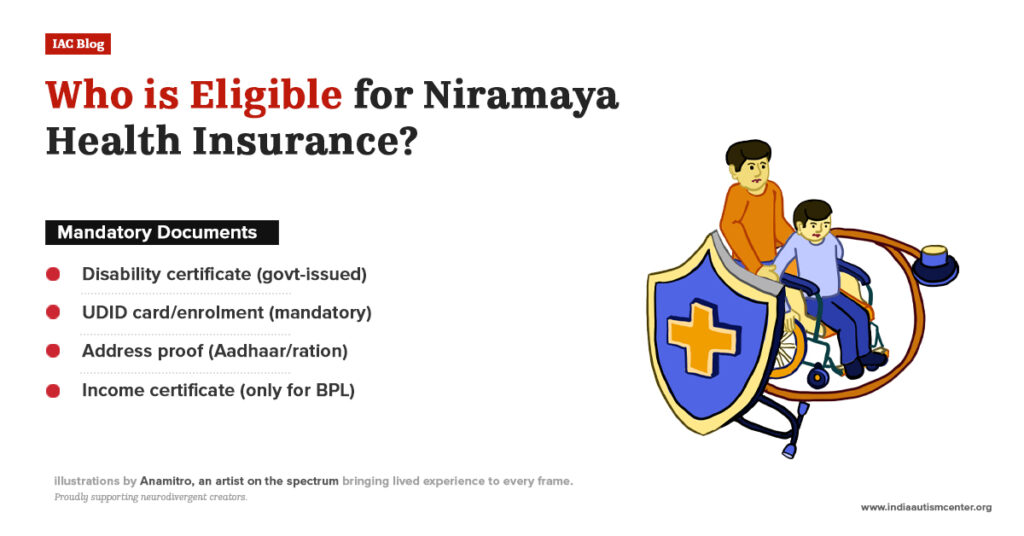
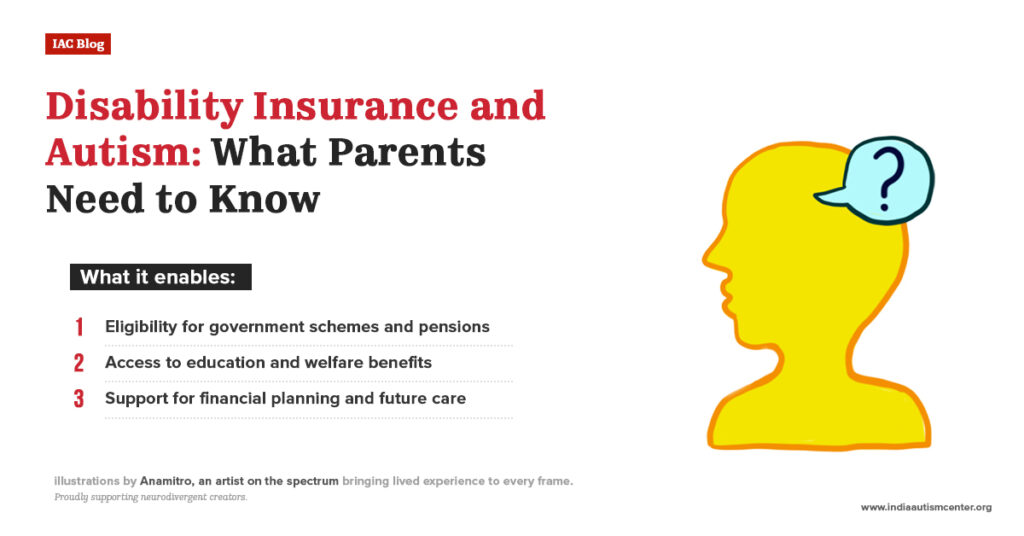
1. Disability Certificate:
- The first step is to obtain a disability certificate from a government hospital or a certified medical authority.
- This certificate is the key to accessing most government schemes.
2. Unique Disability ID (UDID) Card:
- Register for a UDID card. It is a nationwide database and card that simplifies access to benefits.
3. Central Government Schemes:
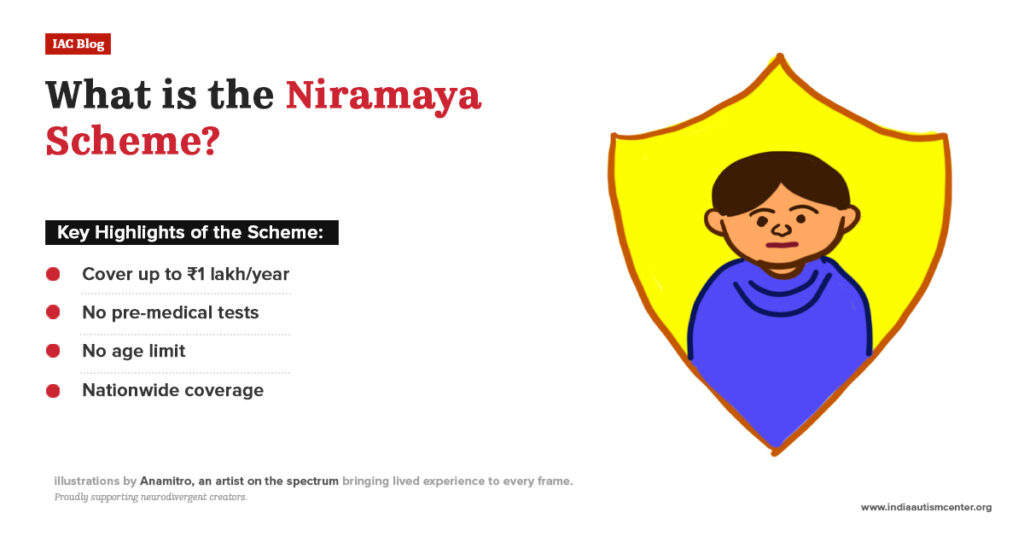
- National Trust Schemes:
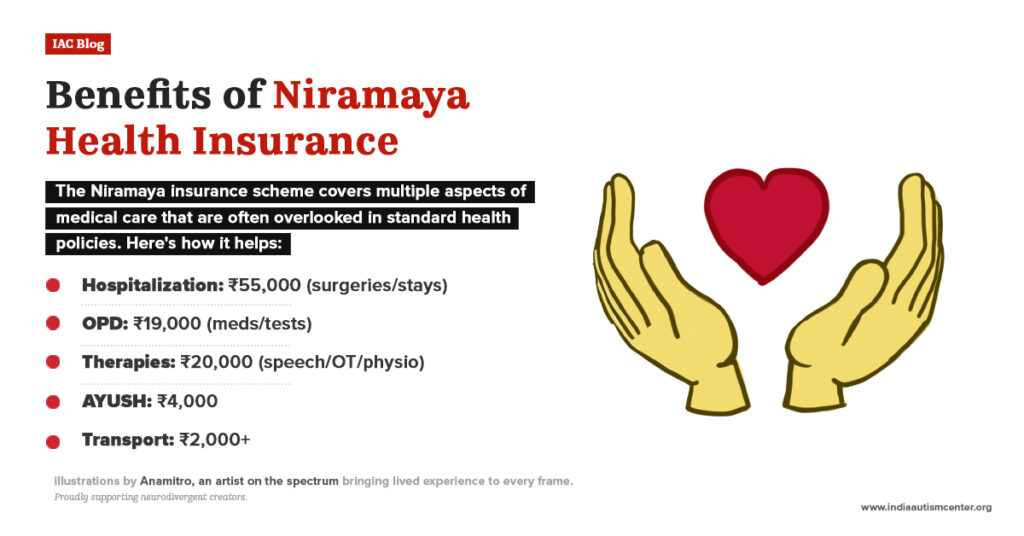
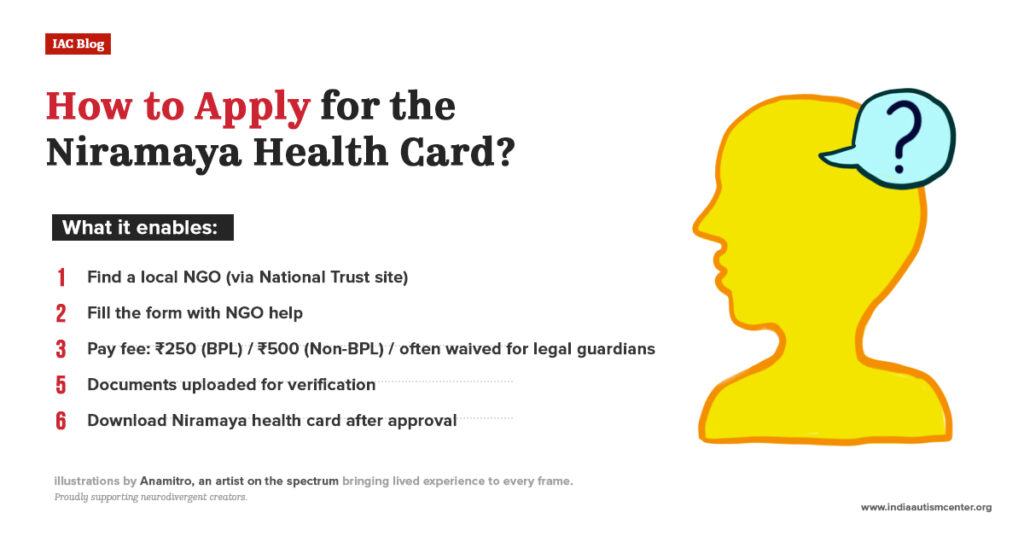
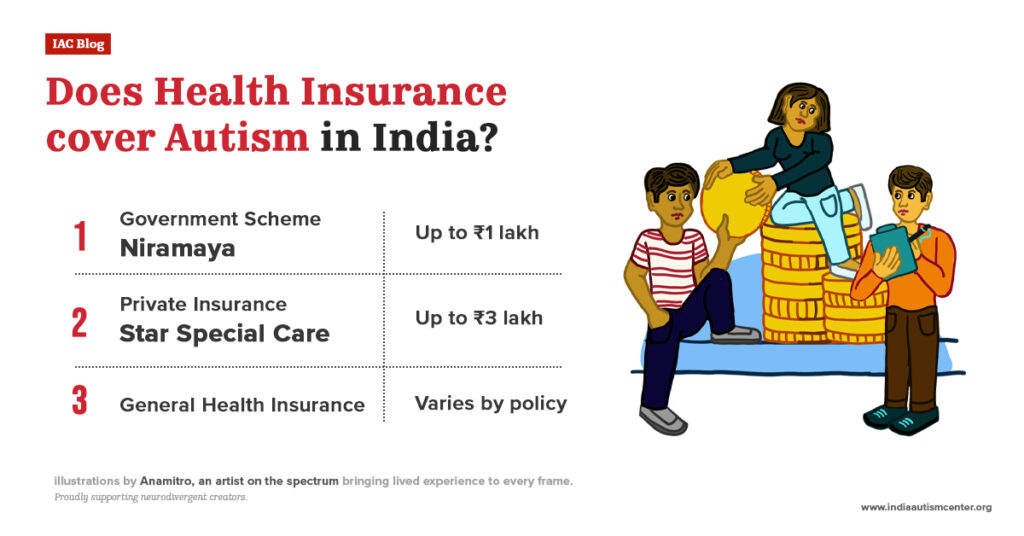
- Niramaya Health Insurance Scheme: Provides health insurance coverage for persons with autism, cerebral palsy, mental retardation, and multiple disabilities. Premium is subsidised. This is a very important scheme to look into.
- Gharaunda (Group Home Scheme): Provides funding for group homes for adults with disabilities.
- Vikaas (Day Care Scheme): Provides day care and respite care for families.
- Samarth (Respite Care Scheme): Provides short-term care to give families a break.
- Scholarships for Persons with Disabilities:
- The Department of Empowerment of Persons with Disabilities (DEPwD) offers scholarships for students with disabilities for school and higher education.
- Income Tax Exemptions:
- Under Section 80DD of the Income Tax Act, you can claim a deduction for expenses incurred on the medical treatment, training, and rehabilitation of a dependent with a disability. The amount depends on the severity of the disability (40% or 80%).
- You can also claim a deduction for payments made to a specified scheme for the maintenance of a dependent with a disability.
- Concessions in Travel:
- Persons with disabilities are often eligible for concessions on Indian Railways and some state transport buses. The disability certificate is required.
4. State Government Schemes:
Each state in India has its own schemes, which may include:
- Monthly pension for persons with disabilities.
- Financial assistance for purchasing assistive devices (tricycles, hearing aids, etc.).
- Marriage assistance schemes.
- Housing schemes.
How to Find Information:
- Visit the website of your State Social Welfare Department.
- Visit the website of the Department of Empowerment of Persons with Disabilities (disabilityaffairs.gov.in).
- Contact local NGOs working in the disability sector. They often have up-to-date information on schemes.
- Approach your local District Disability Rehabilitation Centre (DDRC).
Important: Government schemes change. Benefits you are eligible for today may not exist in 20 years. Do not rely entirely on government support. Use it as a helpful addition to your own savings, not as your main plan.
Part Six: Putting It All Together – Your Action Plan
You have learned a lot. Now it is time to act. Here is a step-by-step plan you can start today.
Phase 1: Immediate Steps (This Month)
- Have the family conversation: Talk to your spouse and close family about long-term plans for your child.
- Track your expenses: Write down every rupee you spend for one month.
- Open a separate savings account: This will be the beginning of your emergency fund.
- Set up a small SIP: Even ₹500 per month in a diversified equity fund is a start.
- Check your insurance: Do you have term life insurance? Health insurance? If not, start researching.
Phase 2: Next 3-6 Months
- Build your emergency fund: Aim for at least 3 months’ expenses, then work toward 6-12 months.
- Apply for a disability certificate and UDID card: If you haven’t already.
- Research government schemes: Find out what your state and central government offer.
- Meet a fee-only financial adviser: Look for one who understands special needs planning. Ask them to help you create a comprehensive plan.
- Meet a lawyer: Discuss writing a will and setting up a trust.
Phase 3: Within the Year
- Write your will: Get it done by a lawyer. Do not delay.
- Set up a trust: If appropriate for your situation, work with your lawyer to create a trust for your child.
- Write your Letter of Intent: Start with a few pages and build on it over time.
- Increase your SIP: If you got a raise, increase your monthly investment amount.
- Review all insurance: Make sure your coverage is adequate.
Phase 4: Ongoing (Every Year)
- Review your financial plan: Set a date each year (e.g., your child’s birthday) to review everything.
- Update your budget: Check if your expenses have changed.
- Adjust for inflation: Increase your savings goals to account for rising costs.
- Review your will and trust: Ensure they still reflect your wishes. Update your Letter of Intent.
- Check your investments: Are they on track? Do you need to rebalance?
- Celebrate your progress: You are doing something incredibly important. Be proud.
Conclusion: You Are Building a Legacy of Love
Financial planning for a child with special needs can feel overwhelming. There are numbers to calculate, forms to fill, and difficult decisions to make. But always remember what this is really about.
You are not just saving money. You are building a future where your child is safe, happy, and loved, even when you are not there. Every rupee you save, every policy you buy, every conversation you have is an act of love.
There will be good days and hard days. Some months you will save more, some months less. That is okay. The important thing is to keep going. Start where you are. Use what you have. Do what you can.
You can do this. And you do not have to do it alone. Reach out to professionals, connect with other parents, and use the resources available.
Your child’s future is bright because you are planning for it.
Please Note: This guide is for educational purposes only and does not constitute financial or legal advice. Please consult qualified professionals for advice tailored to your personal situation. The projections and figures presented in this document are purely illustrative and for planning purposes only. Actual outcomes may differ materially based on market performance, economic conditions, and other prevailing market dynamics.
For expert insights, support services, and inclusive learning initiatives, visit the India Autism Center.