As soon as a child or an adult gets diagnosed with autism, the first question that families ask is how to manage the condition. In India, approximately 1 in 65 children between the ages of two and nine are affected by Autism Spectrum Disorder, with an estimated 1.8 to 2 million children thought to have ASD. The confusion increases as there are multiple therapies for autism treatment available today. Each therapy claims to support development in different ways, and each child responds differently.
From structured interventions like behavioural therapy and speech therapy to creative approaches such as music, art, and play-based therapy, autism therapies serve different purposes at different stages of life.
Understanding the different types of autism therapy is necessary to make an informed decision, as no two autistic individuals need the same type of support.
In this article, we will explain the major categories of autism therapy, how they work, and how they can support long-term progress.
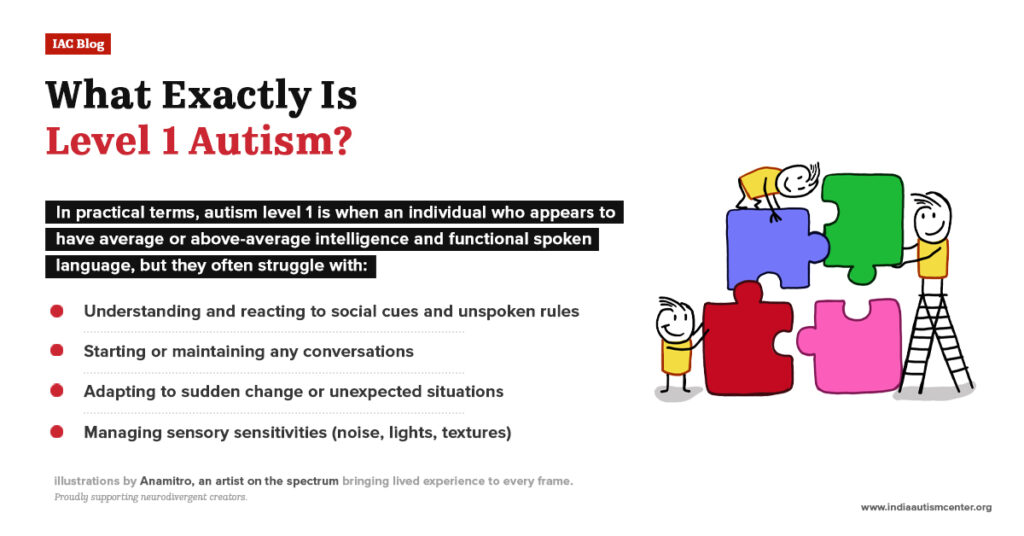
Why Autism Therapy Is Not One-Size-Fits-All?

For parent or family members, it is essential to understand that autism is a spectrum, so:
- No two autistic individuals have the same strengths or challenges.
- There is no fixed timeline for development.
- As the person with autism spectrum disorder ages, the support needs might also change.
So, in reality, there is no concept for fixing autism. It is about supporting communication, building independence, reducing stress, and helping individuals engage with the world in a meaningful and safe way.
Each therapy autism treatment differs from the others in its focus, methods, and outcome. Understanding the key differences assist families to make informed decisions rather than chase every available option.
Broad Categories of Autism Therapies
The autism therapies mostly fall into two overlapping categories, namely:
- Conventional Autism Therapies: These therapies are evidence-based and well-researched, and they form the foundation of most autism intervention programs.
- Non-conventional Autism Therapies: These are complementary or experiential therapies that focus on emotional expression, sensory regulation, creativity, and engagement. They are usually added alongside core therapies.
It is important to know that long-term progress often comes from combining approaches rather than choosing between them.
Conventional Autism Therapies

Conventional autism therapies are the core, evidence-based interventions most commonly recommended to individuals on the spectrum. Instead of addressing autism as a sole challenge, conventional therapies aim to target specific developmental areas, helping individuals function more comfortably and confidently.
Here are some of the conventional therapies that are widely used:
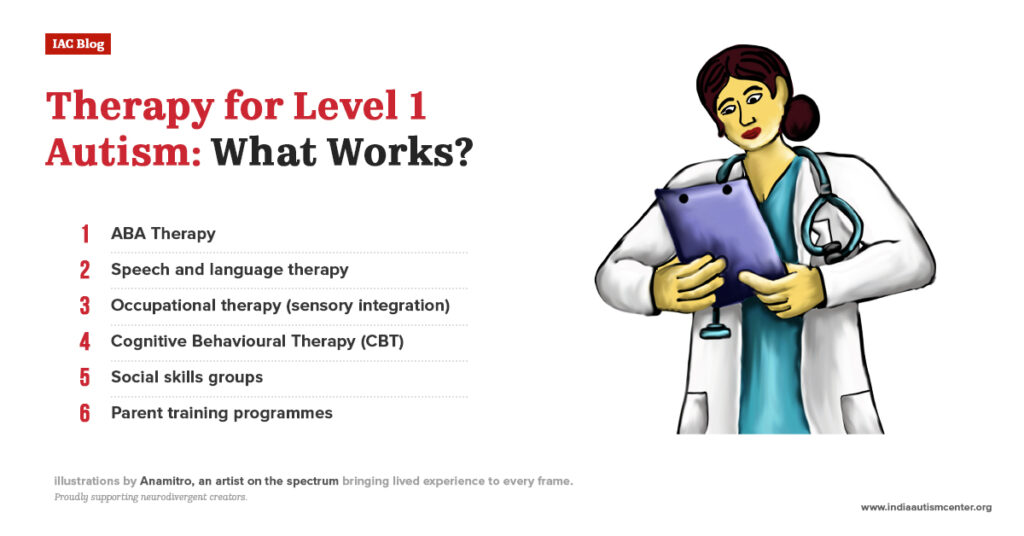
Applied Behaviour Analysis (ABA)
Applied Behaviour Analysis (ABA) is a widely used therapy for autism treatment. It focuses on knowing how behaviour works and using this understanding to:
- Teach new skills to the child with ASD
- Strengthen helpful behaviours
- Reduce behaviours that interfere with learning or daily life
ABA therapy for autism breaks complex skills into small, manageable steps. Each step is taught using repetition, reinforcement, and consistency. The key principles of the ABA therapy for autism include:
- Positive reinforcement can help in encouraging learning
- Data-based decision-making that aims to track progress
- Individualised goal-setting based on the specific needs of an individual on the spectrum.
Although ABA therapy for autism is helpful for people of all ages, it is most commonly used in early intervention and in skill-building for communication, daily living, and learning readiness.
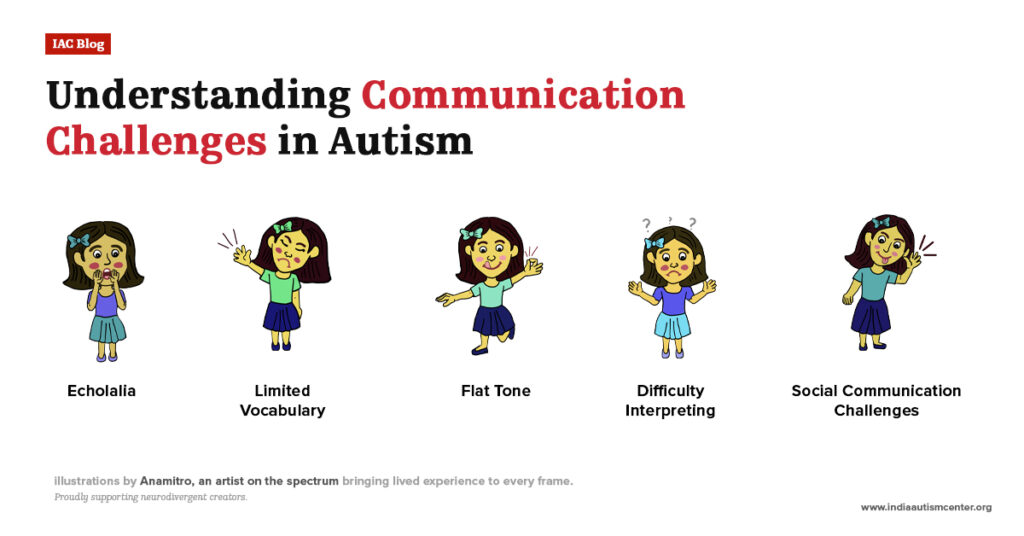
Speech and Language Therapy for Autism
Speech therapy for autism treatment is not only about spoken words, but also about supporting communication in all its forms. Some individuals on the spectrum speak fluently but struggle with social communication; they use limited speech or rely on gestures, visuals, or an assistive device.
The speech-language pathologist works on:
- Expressing needs and emotions
- Understanding language
- Social communication (turn-taking, conversation, nonverbal cues)
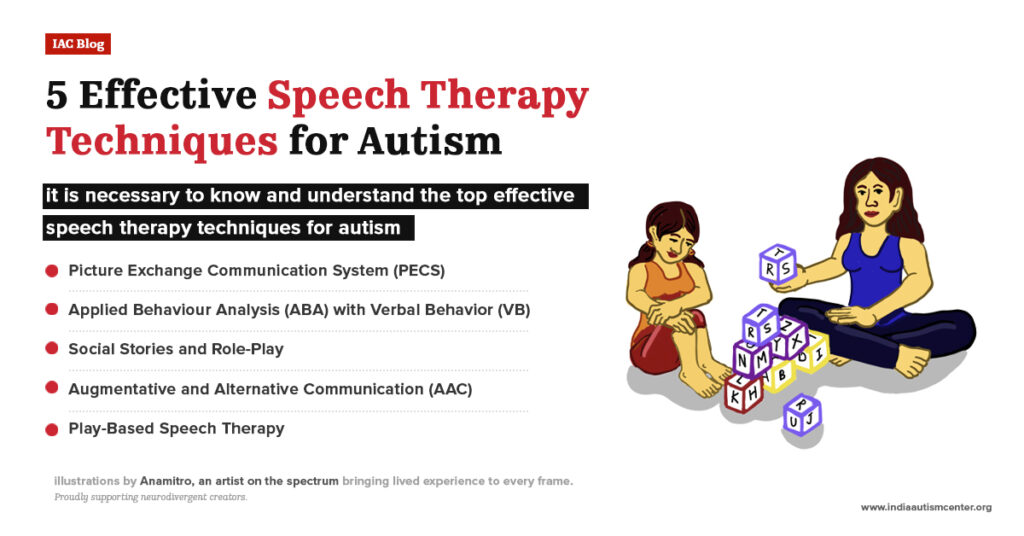
Speech and language therapy also includes Argumentative and Alternative Communication (AAC), visual supports, social stories, and pragmatic language training. The end goal is to improve functional communication.
How speech and language therapy works:
A speech-language pathologist (SLP) starts with the assessment of how the individual communicates across different settings, such as home, school, and social environments. Then, this autism treatment therapy includes:
- Modelling words or gestures either during play or routines
- Using visual aids like pictures or symbols
- Teaching turn-taking and conversational skills through role-play
- Supporting the use of AAC (Augmentative and Alternative Communication) devices
- Practising communication in real-life situations
Speech and language autism therapies can benefit young children with communication issues, children with speech delays, teens, and adults who are working on conversation, self-advocacy, and workplace communication.
Because communication needs change with age, speech therapy can be helpful across the lifespan.
Occupational Therapy (OT) for Autism
Occupational Therapy (OT) helps autistic individuals to take part in everyday activities more comfortably and independently. In this context, “occupation” refers to daily life tasks such as eating, dressing, writing, playing, learning, and managing routines.
For individuals on the spectrum, everyday activities can be quite challenging because of sensory sensitivities, motor skill issues, and planning and transition difficulties. Occupational therapy autism treatment works to reduce these challenges and make daily life feel more predictable and manageable.
Occupational therapy primarily focuses on areas like:
- Daily living skills such as dressing up, feeding, hygiene, and self-care
- Fine motor skills are used to grasp objects, handwriting, and use utensils
- Gross motor skills like balance, coordination, posture, and body awareness
- Sensory regulation, such as managing responses to sound, touch, movement, and visual input
- Emotional regulation, coping with frustration, transitions, and changes in routine
The goal is not to remove sensitivities, but to help the individual respond to sensory input more calmly and effectively. Occupational therapists work as:
- Autism therapy plans which are individualised and not rigid
- Sessions are often play-based and engaging, especially for children
- Strategies are designed to carry over into home, school, and community settings
In the end, it is all about supporting independence, confidence, and active participation in everyday life.
Cognitive Behavioural Therapy (CBT) for Autism
Cognitive Behavioural Therapy for autism focuses on the connection between thoughts, emotions, and behaviours. This is most commonly used with adolescents and adults, or with individuals who can deeply reflect on their thoughts and feelings.
Such autism therapies aim to help individuals on the spectrum understand their emotional responses more easily and develop better coping mechanisms for anxiety, stress and even everyday challenges.
CBT helps to:
- Recognise unhelpful or repetitive thought patterns
- Understand how thoughts influence emotions and behaviour
- Develop practical coping strategies for stress and anxiety
- Improve emotional regulation and self-awareness
- Build confidence in managing social and everyday situations
CBT therapy sessions include:
- Identify challenges like anxiety, anger, or low self-esteem.
- Breaking down the situation that triggers emotional distress.
- Practising alternative, more balanced ways of thinking
- Applying coping strategies in real-life situations
Overall, CBT helps autistic individuals gain greater control of emotional responses, reduce distress, and navigate daily life with increased confidence and resilience.
Non-conventional Autism Therapies

These autism therapies focus on emotional expression, sensory regulation, and engagement through creative and experiential approaches, such as play, music, art, movement, or animal interaction.
Let us look at different non-conventional autism therapies:
Relationship Development Intervention (RDI) for Autism
RDI is all about building emotional connections, flexibility, and shared experiences. So, instead of isolated skill training, RDI focuses on emotional referencing, problem-solving, and adapting to change.
Benefits of relationship development intervention (RDI):
RDI is also instrumental in fine-tuning skills. Besides benefiting children struggling to cope, RDI is also a proven effective autism therapy for adults. This is how:
- Strengthens social connections
- Enhances communication abilities
- Improves emotional regulation
- Fosters independence
- Promotes overall well-being
Parents play a great role in applying strategies during everyday routines. There are different approaches, such as RDI and Floortime, that help children on the spectrum engage more, build stronger emotional connections, and improve social interaction.
They are especially useful for building relationships and social motivation.
Play-Based Therapy for Autism
Play-based therapy for autism uses play as a natural way to build social skills, express emotions, and develop problem-solving abilities. The play can be:
- Child-led
- Structured
- Individual or group-based
Benefits of play-based therapy for autism:
Play-based therapy is a lot of fun. But it definitely has real, tangible benefits:
- Enhances Communication: Children tend to develop better communication skills, including verbal and non-verbal forms, as they express their feelings and engage in play.
- Improves Social Skills: When a child is able to interact with others through play, they learn to share, take turns, and understand social cues, which help them build lasting relationships.
- Builds Emotional Regulation: Through play, children learn to cope with difficult emotions and reduce problem behaviours, allowing them to manage stress and anxiety in an efficient manner.
Such autism therapies help children engage more deeply, as play is meaningful and motivating.
Music Therapy for Autism
This type of therapy for autism uses rhythm, melody, and sound to support communication. Emotional regulation and social interaction. The sessions include:
- Singing
- Instrument play
- Movement to music
- Listening and reflection
Types of Music Therapy for Autism
Music can help us express what’s hard to say, offering comfort, connection, and clarity. In autism treatment therapy, it’s used in two main ways: through active participation or reflective listening.
- Active Music Therapy for Autism: This involves making music with the therapist, including singing, playing instruments, or creating songs together. It’s a hands-on way to explore emotions, build confidence, and strengthen communication.
- Receptive Music Therapy for Autism: In this therapy, the focus is on listening. The child might hear live or recorded music, then talk with the therapist about what it brings up, including memories, emotions, or thoughts. It’s a quieter, reflective path toward understanding and healing.
Music therapy for autism brings spectacular results for individuals who respond strongly to auditory input or struggle with verbal expression.
Art Therapy for Autism
Art therapy for autism focuses on expressing emotions without words. It is done through drawing, sculpting, painting, or collage and helps to:
- Explore emotions
- Reduce stress
- Improve focus
- Build self-esteem
It is helpful for emotional processing, sensory engagement, and self-expression. Here are the benefits of art therapy for autism:
- Stronger bonds with therapist, peers, and family.
- Natural artistic expression will grow, boosting your confidence.
- Fine motor skills will develop through hands-on creativity.
- Better reading and responding to facial expressions.
- Imagination and the ability to think abstractly will expand.
Dance Movement Therapy for Autism
Dance Movement Therapy for autism utilises movement to support body awareness, emotional expression, and social connections. Through various techniques like mirroring, rhythm, and guided movement, individuals on the spectrum can:
- Regulate emotions
- Build confidence
- Feel understood without relying on speech
Various types of dance movement therapy for autism:
- Dance therapy for autism involves using the body to explore emotions, build trust, and feel more at home in one’s own skin. Here are some methods that therapists employ:
- Mirroring: The therapist reflects a child’s movements, which eventually helps to build trust and connection. It helps the child to feel seen without needing to speak.
- Attunement: Children respond to the emotional state with their own movement, helping them feel supported and understood in real time.
- Integrated Development: This method uses movement to work through developmental blocks, whether it is emotional, social, or relational, at the child’s pace.
- Authentic Movement: Children move with their eyes closed, guided by inner cues. The therapist observes, helping them access deeper feelings and early experiences.
Animal-Assisted Therapy for Autism
Animal-assisted therapy for autism uses techniques that involve structured interaction with trained animals. The benefits:
- Reduced levels of anxiety
- Improvement in emotional regulation
- Increased social engagement
Benefits of animal-assisted therapy for autism:
You’ll find a range of powerful benefits for individuals with autism when the autism treatment therapy is administered in a sensory-friendly way through animals.
Here’s how it helps:
- Reduces anxiety: Animals tend to have a very calming presence that helps individuals on the spectrum to manage stress and ease anxiety.
- Improves social skills: When a child on the spectrum interacts with animals, it encourages communication, making it easier to develop social connections and practice essential social cues.
- Boosts emotional well-being: The bond with an animal provides emotional support, fostering increased self-esteem, trust, and a sense of security.
- Encourages physical activity: Caring for or playing with animals promotes movement and physical engagement, improving coordination and motor skills.
There is no judgment from animals, which helps make the therapy feel safer and more motivating.
Home-Based Autism Therapy
Continuing the therapies at home brings better results. Several therapies go beyond session rooms. Home-based therapy includes:
- Parent coaching
- Daily routine-based learning
- Consistency across environments
It is essential to keep it balanced. Avoid overloading your child with too many activities.
Conclusion
When a parent finds that their child is on the spectrum, they start looking for needed support. Since there are so many therapy options, to make an informed decision, it is essential to know the differences between autism therapies and how they work. Each therapy has a distinct purpose; while some therapies aim to build essential life and communication skills, others support emotional regulation, sensory processing, and engagement.
When different therapies are thoughtfully selected, paced well, and tailored to individual needs, they work in unison to support long-term growth, independence, and improvement in overall quality of life.
Frequently Asked Questions
What are the main autism therapies?
Autism therapies are broadly categorised into conventional therapies (such as ABA, speech therapy, occupational therapy, and CBT) and non-conventional therapies (like play therapy, music therapy, art therapy, and animal-assisted therapy). Conventional therapies focus on skill development and daily functioning; on the other hand, non-conventional therapies support emotional regulation, sensory needs, and engagement.
Does therapy really help autism?
Yes, therapy can significantly improve communication, daily living skills, emotional regulation, and independence for autistic individuals. While therapy will not cure autism, it does support meaningful development and improve the quality of everyday life.
Is speech therapy necessary for all autistic children?
Not all autistic children need speech therapy, but many benefit from it. Speech therapy supports both verbal and non-verbal communication, helping individuals express needs, understand language, and improve social interaction in everyday situations.
At what age should autism therapy begin?
Autism therapy can begin as early as toddlerhood, especially when developmental concerns are identified early. Early intervention is beneficial, but therapy can also be effective for older children, teenagers, as well as adults.
Are non-conventional therapies scientifically proven?
Some non-conventional therapies have growing research support, while others are complementary. They are most effective when used alongside evidence-based therapies, not as replacements for core interventions.
Can an autistic child benefit from multiple therapies at once?
More therapy is not always better; it can do more harm than good. Hence, professionals always recommend balancing therapy intensity with the child’s tolerance.
For expert insights, support services, and inclusive learning initiatives, visit the India Autism Center.